Stabilization Before EMDR: A Complete Guide to Building Trauma Resilience
Stabilization forms the foundation of effective Eye Movement Desensitization and Reprocessing (EMDR) therapy. Before diving into trauma processing, clients need a solid base of coping skills, emotional regulation, and internal resources. This comprehensive guide explores Phase 2 of EMDR, providing therapists with the tools to prepare clients for successful trauma resolution.
The Critical Role of Stabilization in EMDR
Why Stabilization Matters
EMDR therapy follows a structured eight-phase protocol, with Phase 2—Preparation—being crucial for treatment success. Without adequate stabilization, trauma processing can lead to:
- Overwhelm: Clients unable to manage emerging emotions
- Dissociation: Loss of present-moment awareness
- Decompensation: Worsening of symptoms
- Dropout: Clients discontinuing therapy prematurely
Stabilization as Capacity Building
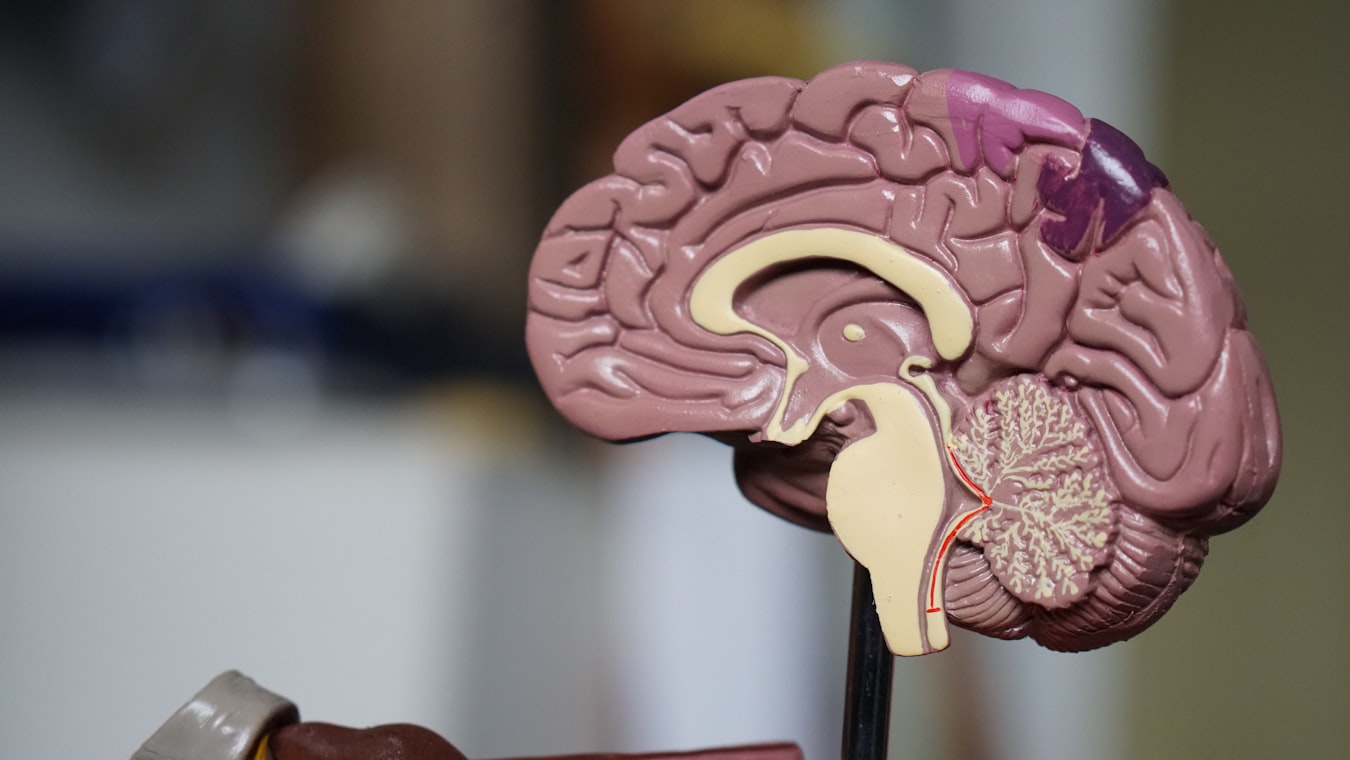
Stabilization strengthens neural pathways for safe trauma processing
Stabilization transforms vulnerability into resilience by:
- Building coping skills: Emotional regulation and distress tolerance
- Developing resources: Internal and external support systems
- Enhancing safety: Creating secure therapeutic foundation
- Preparing the system: Ensuring brain can handle trauma processing
Assessing Stabilization Needs
Client Evaluation
Trauma History Assessment
- Complexity: Single vs. multiple/complex trauma
- Chronicity: Acute vs. long-term trauma exposure
- Current functioning: Daily coping abilities
Risk Factors
- Dissociation: History of dissociative symptoms
- Self-harm: Current or past self-injurious behaviors
- Suicidality: Active suicidal ideation or plans
- Substance use: Active addiction or dependency
Capacity Indicators
Stabilization Readiness Assessment:
━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━
Area | Ready | Needs Work
━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━
Emotional Regulation | Can manage distress | Overwhelmed easily
Coping Skills | Multiple strategies | Few or ineffective
Support System | Reliable network | Isolated/limited
Self-Care | Consistent practices | Neglected/inconsistent
Present Safety | Stable environment | Unsafe conditions
━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━Core Stabilization Techniques
Breathing and Grounding
Diaphragmatic Breathing
- Technique: Slow, deep belly breathing
- Benefits: Activates parasympathetic nervous system
- Practice: 4-count inhale, 4-count hold, 4-count exhale
5-4-3-2-1 Grounding
- 5 things you can see
- 4 things you can touch
- 3 things you can hear
- 2 things you can smell
- 1 thing you can taste
Emotional Regulation Skills
Window of Tolerance
- Concept: Optimal arousal zone for processing
- Hyperarousal: Too activated, needs calming
- Hypoarousal: Too shut down, needs activation
Self-Soothing Techniques
- Physical: Warm blanket, favorite tea, gentle touch
- Sensory: Music, aromas, textures
- Cognitive: Positive affirmations, gratitude practice
Resource Development and Installation (RDI)
Creating Internal Resources
Safe Place Imagery
- Guided visualization: Peaceful, secure location
- Sensory details: Colors, sounds, feelings
- Accessibility: Can access during distress
Nurturing Figures
- Imaginal resourcing: Benevolent, supportive presence
- Qualities: Wisdom, compassion, strength
- Integration: Combines with safe place
Container Exercise
- Mental container: Box/safe to store difficult material
- Boundaries: Can open/close as needed
- Safety: Keeps trauma contained between sessions
Light Stream/Protection Techniques
- Healing light: Flows through body for protection
- Boundaries: Creates protective shield
- Strengthening: Builds internal resilience
Building External Resources
Support Network Development
- Natural supports: Family, friends, community
- Professional supports: Other therapists, support groups
- Crisis resources: Emergency contacts, hotlines
Daily Structure and Routine
- Sleep hygiene: Consistent sleep schedule
- Nutrition: Balanced meals, hydration
- Exercise: Regular physical activity
- Social connection: Meaningful relationships
Phase 2 Implementation
Session Structure
Initial Sessions
- Assessment: Comprehensive evaluation
- Education: Explain EMDR process and stabilization
- Skill building: Teach core techniques
Ongoing Sessions
- Practice: Reinforce learned skills
- Refinement: Adapt techniques to client needs
- Integration: Connect resources to daily life
Client Involvement
- Homework: Practice between sessions
- Self-monitoring: Track stabilization progress
- Feedback: Regular check-ins on effectiveness
Special Populations Considerations
Complex Trauma Survivors
- Extended stabilization: May require months of preparation
- Parts work integration: Address internal conflicts
- Dissociation management: Build tolerance gradually
Children and Adolescents
- Developmental adaptation: Age-appropriate techniques
- Play-based resources: Games, drawings, stories
- Family involvement: Include caregivers in stabilization
Dissociative Clients
- System stabilization: Resources for all parts
- Communication building: Internal dialogue skills
- Gradual exposure: Slow processing introduction
Measuring Stabilization Progress
Quantitative Measures
- SUD baseline: Pre/post stabilization distress levels
- BLAI (Body Sensations): Physical symptom tracking
- Stability scales: Weekly functioning assessment
Qualitative Indicators
- Client reports: "I feel more in control"
- Behavioral changes: Improved daily functioning
- Therapeutic alliance: Increased trust and safety
When to Transition to Processing
Readiness Criteria
- Skill mastery: Can use resources independently
- Emotional stability: Manages distress without decompensation
- Client readiness: Expresses willingness to process
- Safety assessment: No active crisis or high risk
Gradual Transition
- Pilot processing: Brief trials before full sessions
- Resource reinforcement: Continue stabilization during processing
- Flexible pacing: Adjust based on client response
Common Challenges and Solutions
Resistance to Stabilization
- "I want to process now": Educate about necessity
- Impatience: Set realistic timelines
- Secondary gain: Address benefits of remaining unwell
Skill Acquisition Difficulties
- Learning challenges: Simplify techniques
- Trauma interference: Use gentle, non-threatening approaches
- Motivation issues: Connect to client goals
Research Supporting Stabilization
Studies validate Phase 2 importance:
- Cloitre et al. (2010): Skills training enhances trauma treatment outcomes
- Herman (1992): Phase-oriented treatment essential for complex trauma
- Shapiro (2018): Preparation phase prevents processing complications
Meta-analyses show stabilized clients achieve 60-80% better outcomes.
Training and Competence
Required Skills
- Trauma knowledge: Understanding trauma responses
- Skill teaching: Clear instruction and practice
- Resource creativity: Adapt techniques to individual needs
- Pacing expertise: Know when to slow down or advance
Ethical Considerations
- Client autonomy: Respect readiness preferences
- Cultural sensitivity: Adapt to diverse backgrounds
- Safety first: Never rush stabilization
- Competence scope: Refer when beyond skill level
Integration with Treatment Planning
Comprehensive Approach
- Multimodal treatment: Combine with other therapies
- Holistic care: Address physical, emotional, social needs
- Long-term planning: Stabilization as ongoing process
Maintenance and Relapse Prevention
- Ongoing practice: Continue resource use post-processing
- Crisis planning: Emergency stabilization protocols
- Self-care emphasis: Prevent burnout and relapse
Case Study: Effective Stabilization
Client with complex PTSD from childhood abuse.
- Initial assessment: High dissociation, poor coping skills
- Stabilization phase: 12 weeks of resource building
- Techniques used: Safe place, container, breathing skills
- Progress: Reduced daily distress, improved functioning
- Transition: Gradual introduction to processing
- Outcome: Successful trauma resolution with maintained stability
Future Directions
Emerging stabilization approaches include:
- Technology integration: Apps for skill practice
- Virtual reality resources: Immersive safe place creation
- Biofeedback training: Physiological regulation skills
- Cultural adaptations: Traditional healing integration
Conclusion: The Foundation of Healing
Stabilization transforms trauma's aftermath from chaos to manageable challenge. By building a strong foundation in Phase 2, therapists prepare clients not just for EMDR processing, but for a lifetime of resilience. The time invested in stabilization pays dividends in safer, more effective trauma treatment and lasting recovery.
Remember, stabilization isn't just preparation—it's the beginning of healing itself, teaching clients that they have the internal and external resources to face their past and build a brighter future.
References
Cloitre, M., Courtois, C. A., Charuvastra, A., Carapezza, R., Stolbach, B. C., & Green, B. L. (2010). Treatment of complex PTSD: Results of the ISTSS expert clinician survey on best practices. Journal of Traumatic Stress, 24(6), 615-627.
Herman, J. L. (1992). Trauma and recovery: The aftermath of violence--from domestic abuse to political terror. Basic Books.
Shapiro, F. (2018). Eye movement desensitization and reprocessing (EMDR) therapy: Basic principles, protocols, and procedures (3rd ed.). Guilford Press.
This article is for informational purposes only and does not constitute medical advice. EMDR therapy should only be conducted by properly trained and licensed mental health professionals.
Image Credits
- Brain stabilization illustration: Original image from the EMDR therapy project, used under project license for educational content.
- Stabilization readiness diagram: Created using ASCII art for clarity and accessibility.
All content designed to support comprehensive EMDR preparation and safety.