How EMDR Heals Trauma Safely: Understanding the Science and Safety of Trauma Recovery
EMDR safely facilitates trauma healing through evidence-based neurobiological mechanisms
Eye Movement Desensitization and Reprocessing (EMDR) therapy offers a scientifically grounded, safe approach to trauma healing. Understanding how EMDR works and why it's safe can help clients feel confident in their treatment choice. This comprehensive guide explores EMDR's healing mechanisms, safety features, and evidence-based trauma recovery process.
The Foundation: Adaptive Information Processing (AIP) Model
How Trauma Gets Stuck
Trauma Processing:
- Incomplete processing: Trauma disrupts normal memory integration
- Stuck memories: Experiences stored in raw, unprocessed form
- Emotional charge: Intense feelings remain attached to memories
- Maladaptive responses: Survival reactions become generalized
AIP Theory:
- Natural processing: Brain designed to process experiences adaptively
- Trauma interruption: Overwhelming experiences halt processing
- Dysfunctional storage: Memories stored without context or resolution
- Present activation: Current triggers reactivate unprocessed trauma
EMDR's Healing Approach
Restoring Natural Processing:
- Accessing memories: Bringing forth unprocessed trauma safely
- Adding information: Integrating missing context and resources
- Emotional resolution: Reducing distress through reprocessing
- Adaptive storage: Memories stored with appropriate emotional responses
The EMDR Healing Process: Step by Step
Phase 1-2: Preparation and Assessment
Building Safety:
- Therapeutic relationship: Establishing trust and safety
- Resource development: Creating internal and external supports
- Stabilization: Strengthening coping skills and resilience
- Target identification: Selecting appropriate trauma memories
Assessment Tools:
- SUD scale: Measuring current distress levels
- VOC scale: Evaluating belief validity
- Target selection: Choosing optimal processing starting points
Phase 3-6: Processing and Integration
Desensitization (Phase 4):
- Memory activation: Accessing trauma in controlled way
- Bilateral stimulation: Using eye movements, taps, or tones
- Association flow: Following brain's natural processing
- Distress reduction: Gradual decrease in emotional intensity
Installation (Phase 5):
- Positive cognition: Strengthening adaptive beliefs
- Resource integration: Linking positive experiences
- Neural consolidation: Solidifying new learning
- Body scan: Ensuring somatic resolution
Closure (Phase 6):
- Session ending: Safe return to present moment
- Stabilization: Using learned coping skills
- Homework: Between-session practice
- Safety planning: Emergency support access
Phase 7-8: Reevaluation and Integration
Reevaluation (Phase 8):
- Progress assessment: Checking treatment gains
- Residual distress: Identifying remaining issues
- Maintenance planning: Sustaining positive changes
- Follow-up care: Long-term support strategies
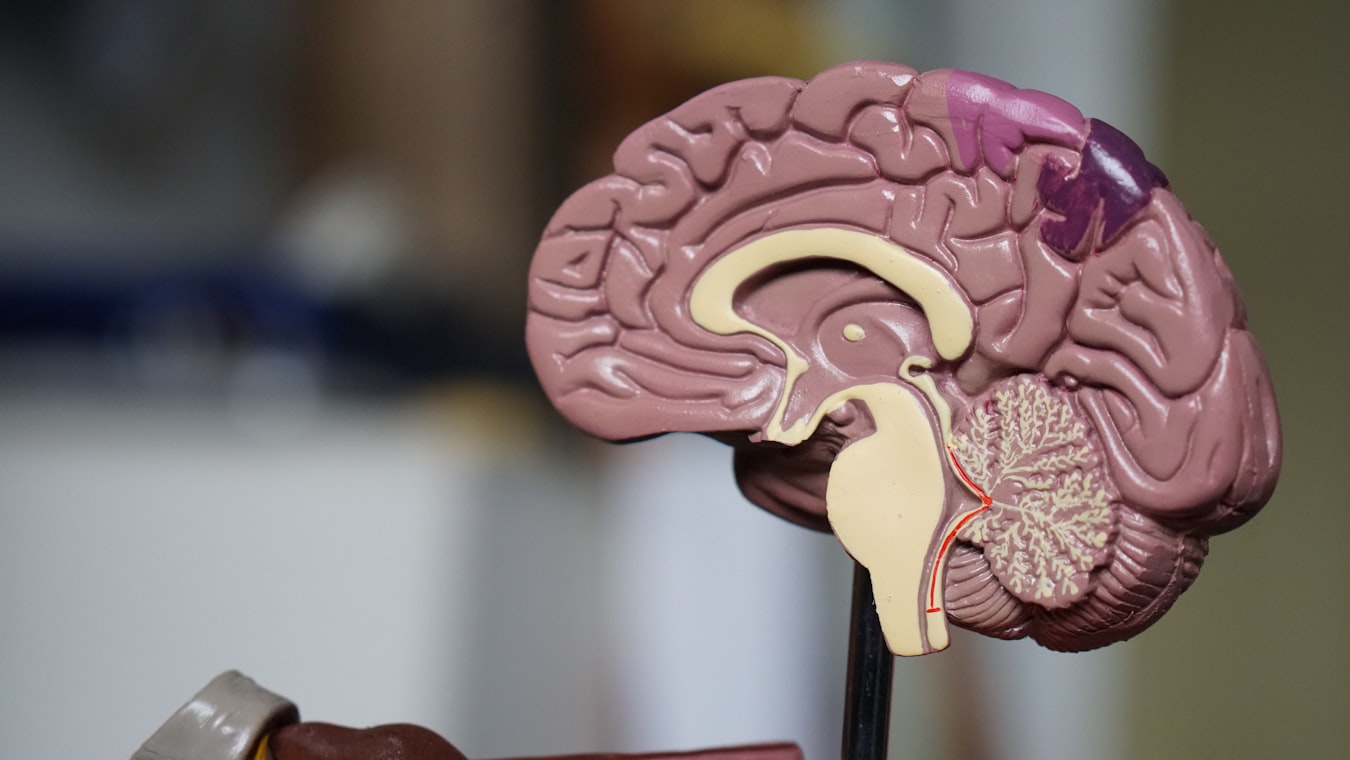
Neurobiological Mechanisms of EMDR Healing
Brain Changes in EMDR
Amygdala Regulation:
- Overactive amygdala: Trauma responses cause hyperarousal
- EMDR modulation: Bilateral stimulation reduces amygdala activity
- Emotional processing: Fear responses become manageable
- Stress reduction: Lower baseline anxiety levels
Hippocampus Integration:
- Memory fragmentation: Trauma disrupts contextual memory
- EMDR reconnection: Bilateral stimulation aids memory integration
- Context restoration: Experiences gain proper time/space context
- Narrative coherence: Trauma stories become integrated
Prefrontal Cortex Strengthening:
- Executive function: Decision-making and emotional regulation
- EMDR enhancement: Improved prefrontal cortex activation
- Cognitive flexibility: Adaptive thinking patterns develop
- Self-regulation: Better emotional control and decision-making
Working Memory Hypothesis
Dual Attention:
- Limited capacity: Brain can only process limited information simultaneously
- Bilateral stimulation: Taxes working memory capacity
- Emotional distance: Creates space from intense feelings
- Adaptive processing: Allows new information integration
Research Evidence:
- fMRI studies: Show reduced limbic system activity
- EEG patterns: Demonstrate brain wave synchronization
- Memory studies: Confirm reconsolidation without strengthening
- Clinical outcomes: Sustained symptom reduction
Safety Features Built Into EMDR
Client Control and Pacing
Voluntary Participation:
- Consent process: Informed decision-making at each step
- Stop signals: Client can pause or end processing anytime
- Pacing control: Speed and depth determined by client comfort
- Boundary setting: Clear limits and safety protocols
Therapist Monitoring:
- Continuous assessment: Checking client state throughout
- Intervention readiness: Prepared for any distress escalation
- Safety anchors: Immediate access to grounding resources
- Post-session support: Between-session safety planning
Gradual Exposure and Titration
Controlled Processing:
- Small chunks: Breaking trauma into manageable pieces
- Resource utilization: Using positive experiences for support
- SUD monitoring: Tracking distress levels continuously
- Flexible pacing: Adjusting based on client responses
Safety Protocols:
- Preparation phase: Building coping skills first
- Resourcing techniques: Creating internal safe places
- Grounding methods: Present-moment orientation skills
- Emergency procedures: Crisis intervention plans
Evidence-Based Safety
Research Validation:
- Low adverse events: Comparable to other trauma therapies
- Predictable responses: Expected reactions well-documented
- Recovery patterns: Most issues resolve spontaneously
- Long-term safety: Benefits outweigh minimal risks
Clinical Standards:
- EMDRIA guidelines: Comprehensive safety protocols
- Training requirements: Rigorous safety education
- Supervision mandates: Ongoing professional oversight
- Quality assurance: Continuous improvement processes
Managing Intensity Safely
Normal Processing Experiences
Expected Sensations:
- Emotional activation: Feelings may intensify then resolve
- Physical responses: Tension, warmth, or energy shifts
- Memory insights: New connections and understandings
- Tearfulness: Emotional release and catharsis
Transient Symptoms:
- Increased dreams: Processing during sleep
- Mild anxiety: Between-session activation
- Body sensations: Somatic processing indicators
- Cognitive shifts: Changing thought patterns
When to Seek Additional Support
Red Flag Indicators:
- Severe dissociation: Complete disconnection from present
- Suicidal ideation: New or increased thoughts
- Self-harm urges: Heightened risk behaviors
- Psychotic symptoms: Hallucinations or delusions
Intervention Strategies:
- Session suspension: Returning to stabilization
- Additional resources: Extra coping skill development
- Collaborative care: Involving other treatment providers
- Modified approach: Adjusting EMDR intensity or pacing
The Role of the Therapeutic Relationship
Safety Through Connection
Alliance Building:
- Trust foundation: Secure attachment for trauma processing
- Empathic attunement: Understanding client experience
- Collaborative process: Shared decision-making
- Consistent presence: Reliable therapeutic contact
Communication Patterns:
- Clear explanations: What to expect and why
- Regular check-ins: Ongoing consent and comfort
- Feedback integration: Using client input to guide process
- Transparency: Open discussion of progress and challenges
Integration with Other Healing Approaches
Complementary Therapies
Holistic Healing:
- Body-based therapies: Somatic experiencing, yoga therapy
- Mindfulness practices: Meditation, breathing exercises
- Creative arts: Art therapy, music therapy
- Movement therapies: Dance therapy, EMDR with movement
Concurrent Treatments:
- Medication management: Psychiatric medication support
- Couples therapy: Relationship trauma processing
- Group therapy: Peer support and validation
- Family therapy: Systemic trauma resolution
Sequential Integration
Phased Treatment:
- Stabilization first: Building foundation before EMDR
- Skills development: Enhancing coping capacities
- Trauma processing: EMDR as primary intervention
- Consolidation: Integration and maintenance phases
Measuring Healing Progress
Objective Indicators
Symptom Tracking:
- PCL-5 reduction: PTSD symptom improvement
- SUD decreases: Distress level monitoring
- VOC increases: Belief change validation
- Functional improvement: Daily life enhancement
Biological Markers:
- Heart rate variability: Autonomic nervous system regulation
- Cortisol levels: Stress hormone normalization
- Sleep quality: Restorative sleep patterns
- Immune function: Overall health improvements
Subjective Experience
Client Reports:
- Emotional relief: Reduced trauma-related distress
- Cognitive shifts: Changed thinking patterns
- Behavioral changes: Improved daily functioning
- Relationship improvements: Better interpersonal connections
Qualitative Changes:
- Meaning making: Understanding trauma's impact
- Self-compassion: Reduced self-blame and judgment
- Future orientation: Hope and goal-directed thinking
- Resilience building: Enhanced coping capacities
Long-Term Healing Benefits
Sustained Recovery
Lasting Changes:
- Memory reconsolidation: Permanently altered trauma storage
- Neural plasticity: Brain rewiring for adaptive responses
- Emotional regulation: Improved affect tolerance
- Relationship patterns: Healthier attachment styles
Preventive Effects:
- Future resilience: Better handling of new stressors
- Symptom prevention: Reduced vulnerability to re-traumatization
- Health improvements: Physical and mental well-being
- Life satisfaction: Enhanced quality of life
Conclusion: Safe, Effective Trauma Healing
EMDR therapy heals trauma safely through scientifically validated mechanisms that respect the brain's natural processing capacities. The therapy's built-in safety features, combined with professional oversight and client control, ensure that healing occurs at a manageable pace with minimal risk.
Understanding EMDR's healing process can help clients approach treatment with confidence, knowing that the intensity they may experience is part of a carefully orchestrated path to recovery. EMDR doesn't just reduce symptoms—it fundamentally changes how trauma is stored and experienced, leading to lasting healing and growth.
References
Shapiro, F. (2018). Eye movement desensitization and reprocessing (EMDR) therapy: Basic principles, protocols, and procedures (3rd ed.). Guilford Press.
Solomon, R. M., & Shapiro, F. (2008). EMDR and the adaptive information processing model: Potential mechanisms of change. Journal of EMDR Practice and Research, 2(4), 315-325.
van der Kolk, B. A. (2014). The body keeps the score: Brain, mind, and body in the healing of trauma. Viking.
This article is for informational purposes only and does not constitute medical advice. EMDR therapy should only be conducted by properly trained and licensed mental health professionals.
Image Credits
- Brain healing mechanisms illustration: Original image from the EMDR therapy project, used under project license for educational content.
- EMDR safety features diagram: Created using ASCII art for clarity and accessibility.
All content designed to explain EMDR's safe trauma healing process.