Dissociation and EMDR: A Complete Guide to Safe Trauma Processing
Dissociation presents both challenges and opportunities in Eye Movement Desensitization and Reprocessing (EMDR) therapy. While EMDR can effectively process trauma that underlies dissociative symptoms, it requires careful assessment and management to ensure safety. This comprehensive guide explores dissociation in the context of EMDR, providing therapists with the knowledge and tools to work effectively with dissociative clients.
Understanding Dissociation in Trauma
What is Dissociation?
Dissociation is a complex psychological process where a person disconnects from their thoughts, feelings, memories, or sense of identity. It's the brain's protective response to overwhelming trauma, creating distance from unbearable experiences.
Types of Dissociation
Detachment Dissociation
- Depersonalization: Feeling detached from oneself ("I feel like I'm watching myself")
- Derealization: Feeling detached from surroundings ("The world feels unreal")
- Emotional numbing: Loss of emotional responsiveness
Compartmentalization Dissociation
- Dissociative amnesia: Memory gaps for traumatic events
- Fragmented identity: Parts of self operating independently
- Compartmentalized memories: Trauma stored separately from daily functioning
Dissociation as a Trauma Response
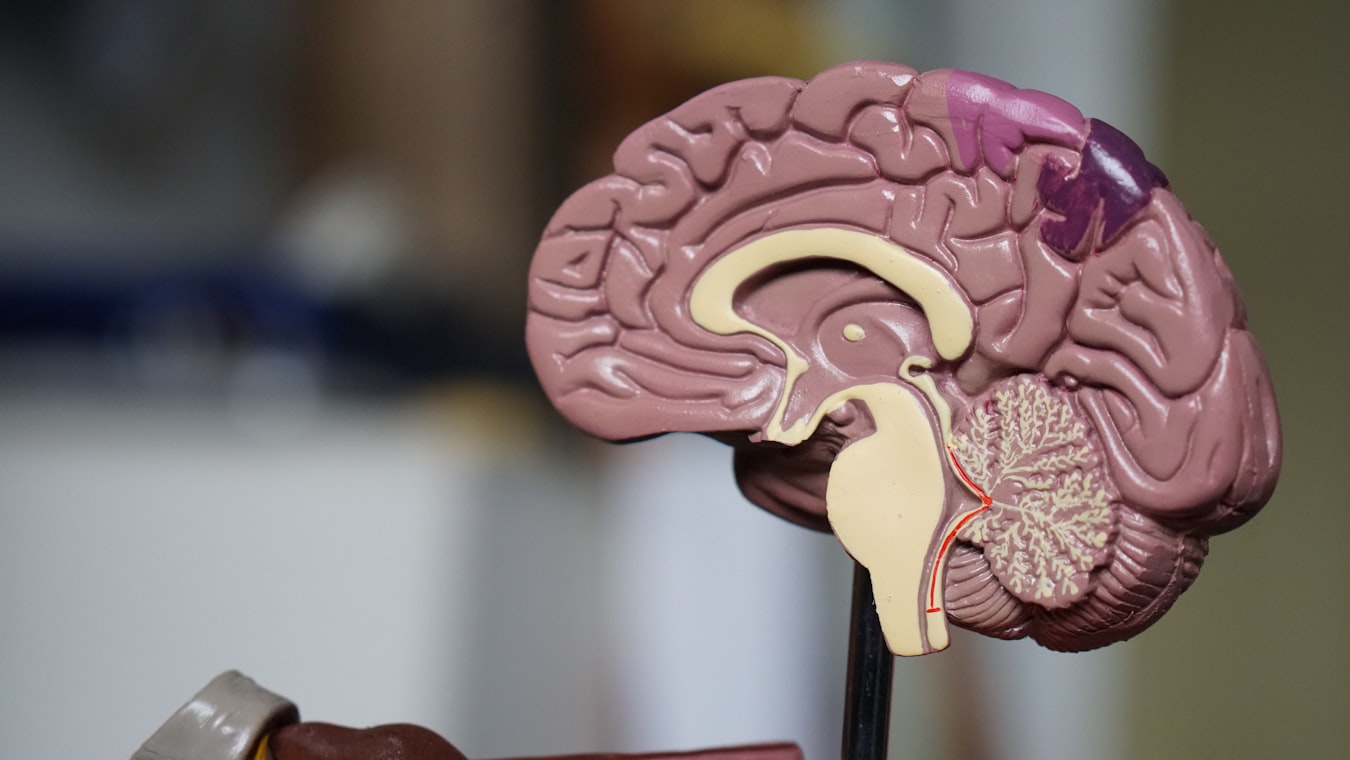
Dissociation as the brain's protective response to overwhelming trauma
Dissociation develops as:
- Survival mechanism: Allows functioning during trauma
- Adaptive response: Protects psyche from overwhelm
- Neurobiological adaptation: Alters brain processing to manage threat
Dissociation and EMDR Processing
How EMDR Affects Dissociation
EMDR can both trigger and resolve dissociative symptoms:
Potential Risks
- Increased dissociation: Processing may temporarily heighten symptoms
- Fragmentation: Accessing dissociated parts without integration
- Overwhelm: Bilateral stimulation too intense for fragile clients
Therapeutic Benefits
- Integration: Links dissociated parts and memories
- Resolution: Processes trauma underlying dissociation
- Stabilization: Reduces need for dissociative defenses
When Dissociation Occurs in EMDR
Normal Processing Dissociation
- Brief detachment during intense processing
- Resolves spontaneously
- Indicates active reprocessing
Problematic Dissociation
- Prolonged disconnection
- Client unable to engage
- Increased fragmentation
Assessment of Dissociative Capacity
Pre-Treatment Evaluation
Dissociation Screening
- DES (Dissociative Experiences Scale): Measures dissociative tendencies
- MID (Multidimensional Inventory of Dissociation): Assesses dissociative structure
- Clinical interview: History of dissociative symptoms
Trauma History Assessment
- Complex trauma indicators: Multiple traumas, early onset
- Attachment disruptions: Insecure or disorganized attachment
- Developmental trauma: Childhood abuse or neglect
In-Session Monitoring
Ongoing Assessment
- Client reports: "I feel spaced out," "I feel detached"
- Behavioral cues: Blank stares, delayed responses, confusion
- Physiological signs: Dissociated breathing, lack of body awareness
Dissociation Levels
Dissociation Continuum in EMDR:
━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━
Level | Indicators | Intervention
━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━
Mild (Normal) | Brief detachment, returns quickly | Continue processing
Moderate | Spaced out, partial engagement | Grounding techniques
Severe | Complete disconnection, confusion | Stop processing, stabilize
━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━Preparation for EMDR with Dissociative Clients
Phase 2 Modifications
Enhanced Stabilization
- Grounding skills: Body awareness, present-moment focus
- Resource development: Safe place, container exercises
- Parts work education: Understanding internal system
Building Dissociation Tolerance
- Gradual exposure: Start with less intense material
- Pacing control: Client-directed speed
- Safety signals: Stop/start cues
Resource Installation
Dissociation-Specific Resources
- Grounding anchors: Physical objects, sensory cues
- Internal safe places: Accessible even when dissociated
- Parts communication: Ways to connect dissociated aspects
Managing Dissociation During EMDR
Immediate Interventions
Light Dissociation
- Continue processing: Often resolves naturally
- Verbal anchoring: "Stay with me here"
- Bilateral stimulation adjustment: Slower pace
Moderate Dissociation
- Grounding techniques: "Feel your feet on the floor"
- Breathing exercises: "Take a deep breath with me"
- Return to present: "What do you notice in the room right now?"
Severe Dissociation
- Stop processing: Return to stabilization
- Reorientation: "You're safe here, in my office"
- Parts work: "Which part is present now?"
Long-Term Management
Integration Strategies
- Parts mapping: Identify and connect dissociated aspects
- Memory linking: Connect fragmented trauma memories
- Identity consolidation: Build cohesive sense of self
Special Considerations for DID/OSDD
Working with Dissociative Identity Disorder
System Assessment
- Parts identification: Who is present, their roles
- Cooperation level: Willingness to work together
- Internal communication: How parts interact
Treatment Modifications
- Part-specific processing: Work with individual alters
- System agreements: Consent and cooperation protocols
- Integration pacing: Gradual unification process
Ethical Considerations
- Informed consent: Explain dissociation risks and benefits
- System consent: Get agreement from all parts when possible
- Boundaries: Clear therapeutic frame for complex systems
Research and Efficacy
Studies support EMDR's effectiveness with dissociative clients:
- Boon et al. (2011): EMDR reduces dissociative symptoms in DID
- van der Hart et al. (2006): Phase-oriented treatment essential
- Schnyder et al. (2015): EMDR superior to waitlist for complex PTSD
Meta-analyses show 70-80% improvement rates with proper dissociation management.
Training and Competence
Required Skills
- Trauma expertise: Understanding complex trauma
- Dissociation knowledge: Assessment and intervention
- Stabilization techniques: Resource installation, grounding
- Integration methods: Parts work, memory linking
Supervision Needs
- Complex cases: Regular consultation for DID/OSDD
- Stuck processing: Dissociation-related blocks
- Ethical dilemmas: Consent and boundary issues
Cultural and Individual Factors
Cultural Considerations
- Cultural dissociation: Normal in some cultures (e.g., possession states)
- Stigma: Mental health stigma affecting disclosure
- Healing beliefs: Cultural models of trauma and recovery
Individual Differences
- Resilience factors: Support systems, coping skills
- Trauma load: Number and severity of traumas
- Developmental stage: Age of trauma onset
Integration with Other Therapies
Complementary Approaches
- DBT: Skills for emotion regulation and dissociation
- Somatic therapies: Body-based stabilization
- Psychodynamic therapy: Understanding dissociative structure
Sequential Treatment
- Stabilization first: Build capacity before trauma processing
- Integrated approach: Combine therapies for complex cases
- Maintenance: Ongoing support during EMDR
Case Study: EMDR with Dissociation
Client with DID processing childhood abuse.
- Preparation: 6 months stabilization, parts mapping
- Initial dissociation: Severe during first session
- Management: Stopped processing, used grounding, parts communication
- Gradual progress: Started with less threatening memories
- Outcome: Reduced switching, integrated trauma memories, improved functioning
Future Directions
Emerging approaches include:
- Neurofeedback integration: Real-time dissociation monitoring
- Virtual reality resources: Immersive grounding techniques
- AI-assisted tracking: Pattern recognition for dissociation risk
- Cultural adaptations: Culturally sensitive dissociation interventions
Conclusion: Dissociation as a Path to Integration
Dissociation, while challenging, represents the brain's attempt to protect itself from trauma. With careful assessment and skilled intervention, EMDR can help dissociative clients achieve integration and healing. The key lies in respecting dissociation as a survival strategy while gently guiding toward adaptive processing.
When approached with knowledge, compassion, and skill, EMDR becomes a powerful tool for resolving even the most complex dissociative presentations, transforming fragmentation into wholeness.
References
Boon, S., Steele, K., & van der Hart, O. (2011). Coping with trauma-related dissociation: Skills training for patients and therapists. W. W. Norton & Company.
Schnyder, U., Ehlers, A., Elbert, T., Foa, E. B., Gersons, B. P., Resick, P. A., ... & Cloitre, M. (2015). WHO guidelines for the management of conditions specifically related to stress. World Health Organization.
Van der Hart, O., Nijenhuis, E., & Steele, K. (2006). The haunted self: Structural dissociation and the treatment of chronic traumatization. W. W. Norton & Company.
This article is for informational purposes only and does not constitute medical advice. EMDR therapy should only be conducted by properly trained and licensed mental health professionals.
Image Credits
- Brain dissociation illustration: Original image from the EMDR therapy project, used under project license for educational content.
- Dissociation continuum diagram: Created using ASCII art for clarity and accessibility.
All content designed to support safe EMDR practice with dissociative clients.